Helping patients and families
- Representative of patients’ organisations
- Patients Committee
- EU added value
- Cross-border healthcare services
Patients are represented in TransplantChild through the Patients Sub-committee, which is constituted by a representative named by the Patients Associations and Advocated Organisations collaborating with the ERN. The Chair of the Patient Committee is part of the Board of the Network for:
- Inform about activities and relevant outcomes of the Patients Committee
- Provide patients and families point of view
- Suggest relevant issues that can be carried out by the ERN
Identify and suggest expert centres or other healthcare professionals that should join the ERN
TransplantChild Patients Committee is composed by:
- Members: a representative of each patients association or advocacy group related to paediatric transplantation in Europe. All organisations are invited to join.
- Chair: the committee members shall appoint one of the members for a period of two years.
- Coordinator: one member of the EOC acts as Coordinator to facilitate the development of SubCommittee proposals as well as to ensure consistency in the development of the Network.
Patients Committee responsabilities:
The Patients Committee is aimed at providing the framework to take into consideration patients and their families’ voice and experience, by:
- Proposing, to the Executive Operating Committee, relevant issues to ensure patient involvement in the development of the Network in aspects such as:
- Patient information, education and training activities for patients and families, good practice guidelines, treatment and care pathways for professional advice.
- Inform about patients needs and gaps in order to prioritise if possible research in these areas.
- Ethical issues on the application of personal data law, compliance of informed consent and patients ´rights.
- Attending to the Working Groups meetings in which the patients representatives participate
- Supporting the network with the dissemination of information and communication to the wider European patient community.
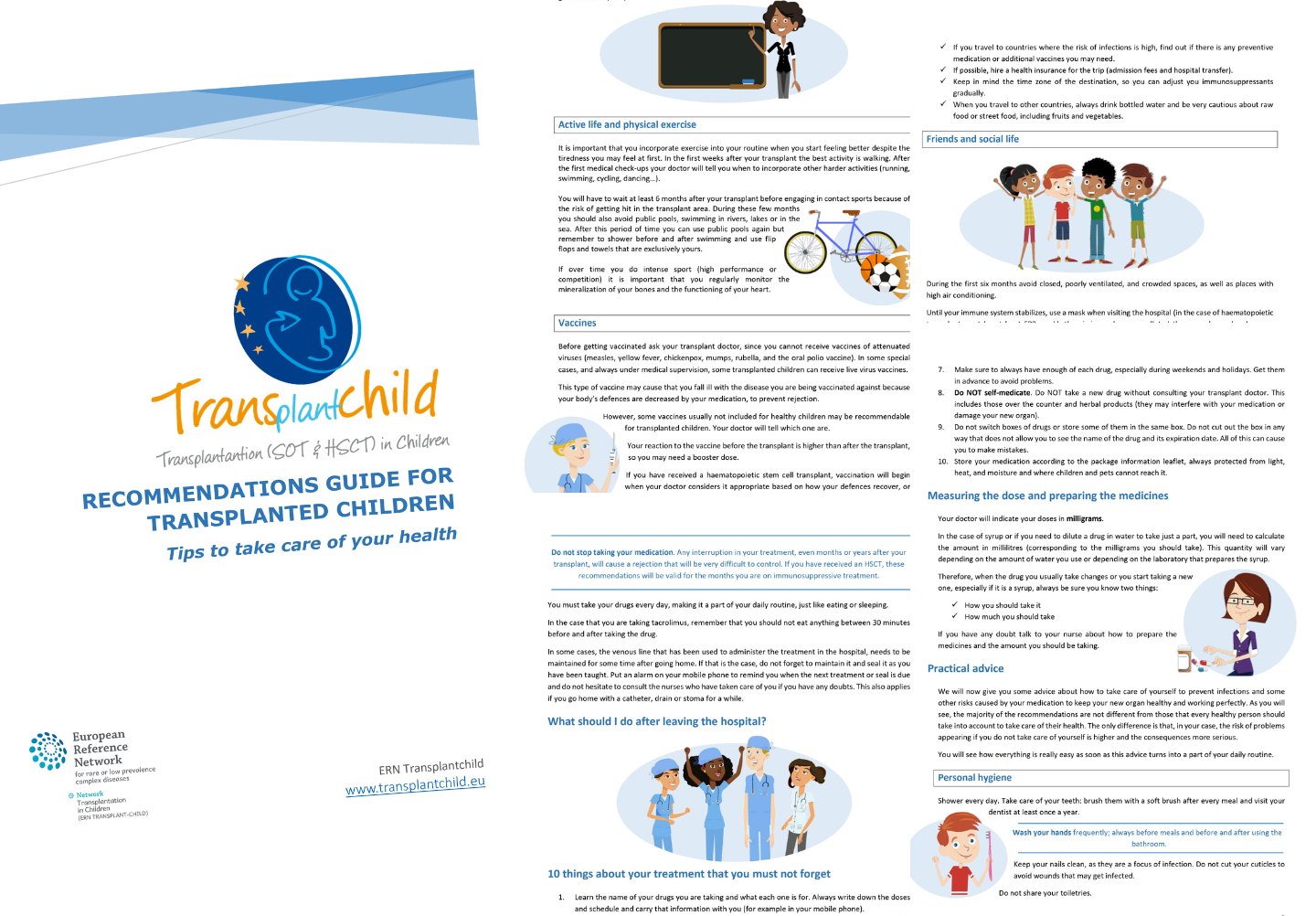
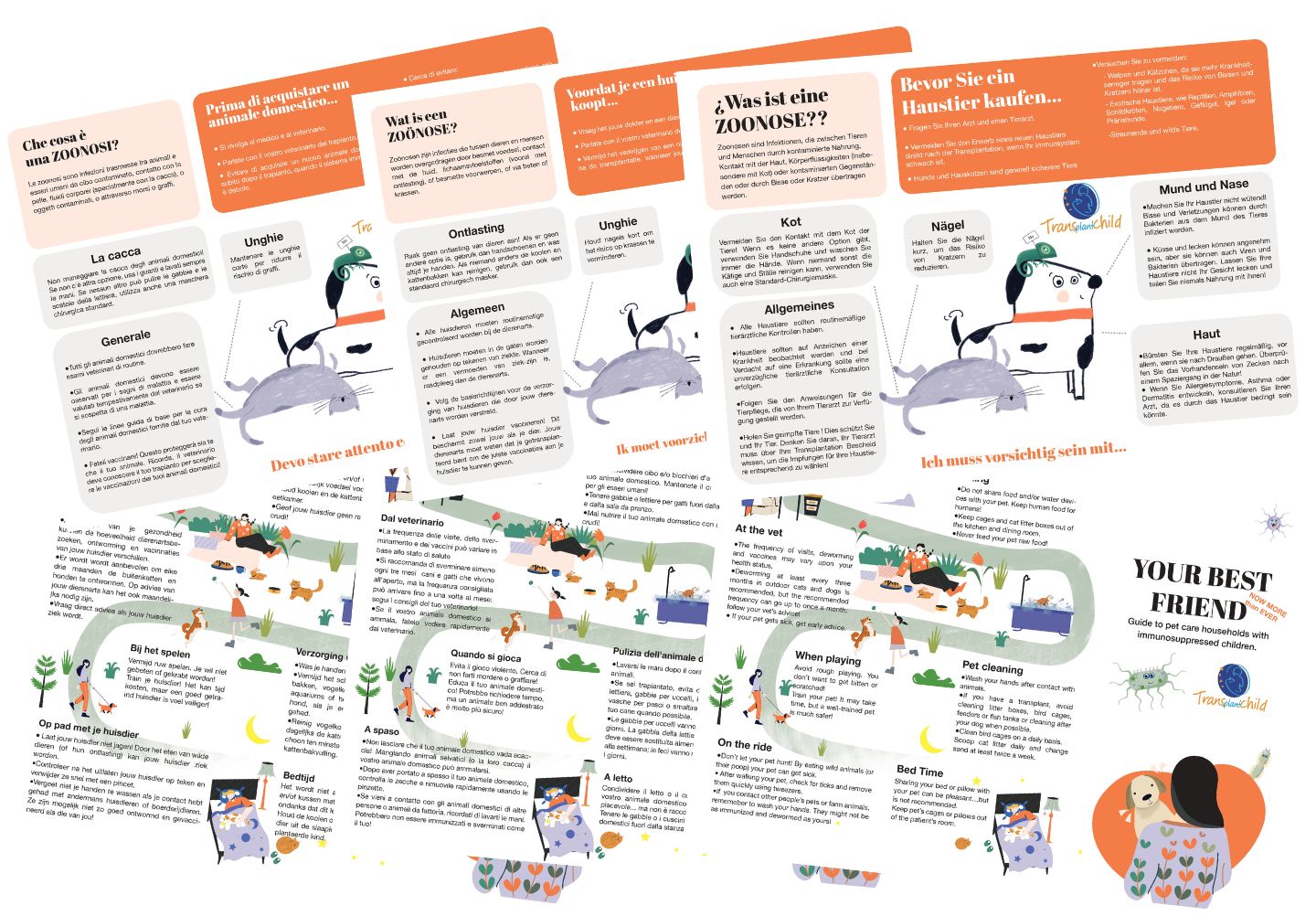
TransplantChild strives to increase life expectancy and quality of life of paediatric patients requiring a solid organ or hematopoietic progenitor transplantation and their families, and will provide added value to patients, families and patients’ organizations, by:
- Involving and giving a voice to families and patients’ organizations and increasing social awareness;
- Facilitating awareness, self-control, training and participation of the patient/family in the care of their condition;
- Making available the latest knowledge in medical, pharmacological and therapeutic advances;
- Providing psychosocial support to children during school age and in their transition to adulthood;
- Providing information about available clinical trials and research projects;
- Reducing hospitalisation time and the use of complex and long-lasting treatments and humanising paediatric care in the hospital units.
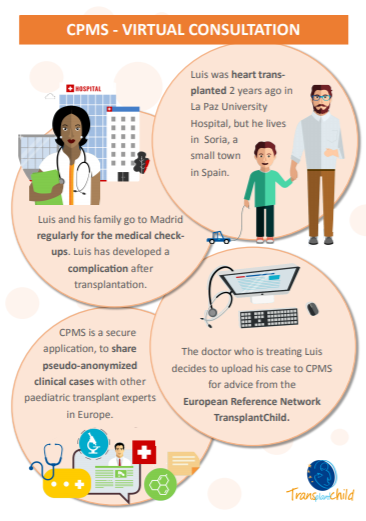
In relation to the implementation of Directive 2011/24/EU on the application of patients’ rights in cross-border healthcare, ERN TransplantChild offers the following services and information:
- Expert virtual clinical advice on the entire transplant process through the Clinical Patient Management System (CPMS). Organ access and allocation are not included in the network’s services.
ERNs are not directly accessible to individual patients/families. However, with the patients’ consent and in accordance with the rules of their national health system, patient case can be referred to the centre/s involved in TransplanChild in their country by their local hospital.
For additional information about cross-border care for patients when travelling/living in another EU country, visit “Your Europe” website: https://europa.eu/youreurope/citizens/health/index_en.htm
PROMs and PREMs
Transplantchild truly believes in the need to care and treat patients in a special way, attending to their special needs as children. Listening to their opinions and experiences and making them part of the network.
ERN TransplantChild will use the patient’s opinions integrated with the clinical data in the PaEdiatric Transplant European Registry (PETER)
INVISIBLE
PROMs
Patient-reported outcome measures (PROMs) are defined as standardized, validated questionnaires (which are also called instruments) completed by patients to measure their perception of their functional well-being and health status.
PREMs
Patient-reported experience measurements (PREMs) are clinical tools used to collect information reported by patients related to their satisfaction about the health system.

PREMs Workshop with TransplantChild Patient Associations Representatives in Padova 2019.
FREQUENTLY ASKED QUESTIONS
TransplantChild answers the most common question of the process of transplantation in children
FAQs brochure

INVISIBLE
What is a transplant?
A transplant is an operation in which a healthy organ or tissue of a donor is implanted into a person or recipient that has an irreversible malfunction of that organ.
Who needs a transplant?
A transplant is needed by a person with permanent and irreversible damage to an organ or tissue, which causes disability, reduces their quality of life and can cause death.
What is the purpose of a transplant?
Who has access to a transplant?
People with irreversible and permanent damage in one of their organs or tissues that have no alternative to medical and surgical treatment. In those cases, a transplantation is the only solution to avoid death or to improve quality of life. This person must undergo a rigorous study and meet criteria evaluated by a group of specialists. The process of donation is always altruistic, confidential and regulated.
What problems can be expected?
The main problem after transplantation is rejection. Our body has an innate response of the cells to reject what is not their own, so it is necessary to give drugs to reduce that immune response. This makes the patient more susceptible to infectious diseases and some tumors or cancer.
Piercing and tattooing?
Piercing or tattooing requires an injury in the skin, so it is not recommended to enhance them in trasnplanted patients due to the risk of infection. In case the patient decides to get them despite the warning, it should be with prior knowledge of their group of physicians and should be done with certified professionals using sterile and disposable materials.
How long will the transplant last?
In kidney grafts involving identical twins, in which case rejection is not a problem, recipients have survived more than 25 years. A number of patients who have received kidneys from unrelated cadaver donors have survived more than 20 years, demonstrating that in some patient’s rejection can be controlled with standard immunosuppressive drugs. There has been a gradual improvement in the overall results of kidney transplants. Liver transplant can have excellent outcomes. Recipients have been known to live a normal life over 30 years after the operation. Transplant recipients directly contribute to the success of their transplant. Failure to comply with the immunosuppressive medical regimen is the first cause of organ failure. Close follow-up with your transplant team and primary-care physician can help ensure a good outcome.
What are the immunosuppressive medicines?
After a transplantation, differences in donor and recipient tissues can cause the body’s defensive system to react by recognizing the “new” organ as foreign. This can cause a failure of the transplanted organ, called “rejection”. To avoid this, the patient must take a medication that reduces the risk of rejection, called immunosuppressive treatment. In transplanted patients, the immunosuppressive treatment diminishes the capacity of the organism to react against cells of the transplanted organ, therefore, are used as prevention and treatment of the rejection. Those drugs are taken from the first day after transplant and during all life to prevent rejection of the transplanted organ.
Why immunosuppression avoids rejection?
Immunosuppressants use heterogeneous mechanisms of action to suppress the body’s cell-mediated and humoral immune response. By weakening or reducing your immune system’s responses to foreign material, these drugs reduce your immune system’s ability to reject a transplanted organ. These drugs also allow you to maintain enough immunity to prevent overwhelming infection. Many of the medications used to achieve immunosuppression have adverse effects of their own.
Will I need to have medication during all my life?
Organ transplantation is successful because of the attenuating effect of immunosuppressive drugs on host immune responses to the graft. Initially, while the risk of rejection is greatest, a higher level of immunosuppression is required. After several months, however, the organ, the host, or both adapt: the host becomes less responsive while the organ loses its population of donor antigen presenting cells. The tendency of the host to mount a rejection response against the graft is diminished, allowing the level of immunosuppression to be reduced after several months. This state of partial adaptation requires continuous presence of the graft and, in most cases, continued immunosuppression.
What are the effects of immunosuppression?
Side effects of the specific medication of the transplant are: decrease of defenses, with increased risk of infections and exceptionally, the appearance of tumors. Other side effects include: hypertension, diabetes, diarrhea, neurological problems, elevation of cholesterol and triglycerides, as well as osteoporosis. In most cases these complications are resolved with medical treatment.
How can I explain to my children that he/she needs a transplant?
The message should be simple, adapted to their age and previous experience with illnesses, and they should have the opportunity to ask questions. They usually understand that some piece of the body (organ) is sick and it needs to be replaced. Many of them ask where the organ comes from, and we should explain the process of cadaveric donation, and living donations if that is the case, and we would emphasizes the generosity and the positive experience of sharing life. Before transplantation, the family will need some visits or even to stay for a while at the hospital. It is important to explain the kids that they will meet many children with similar problems, and staff people that will take care of them.
Who may be candidate to a transplant?
Transplantation can be indicated in cases of irreversible organ failure, when conservative treatments are exhausted or not available. The solid organs that can be currently transplanted in children are: kidney, liver, heart, intestine and lung. Apart from solid organs, bone marrow and other tissues can also be transplanted: heart valves, skin, bone, etc. In spite of the need of organ replacement, transplantation might be contraindicated in a minority of children with oncological diseases, sepsis or critical state. Every case requires individual evaluation.
How is a transplant developed?
After the positive evaluation, the child becomes a candidate for transplantation and is included in the so-called waiting list. Then, they have to wait, usually at home, until they receive the call telling that a suitable organ is available. The “call” is unexpected and can be in the middle of the night, the family is asked to go to the hospital by car or ambulance while some part of the surgical team travel to perform the donor procedure. When the family arrives, the child is prepared to go to the operating room and the recipient procedure stars. When the procurement team arrives, they do the back table procedure, consisting in preparing the organ to be implanted. Finally, the corresponding native organ is removed and the new organ (graft) is implanted.
How long does the surgery takes?
It depends on the organ and the previous surgical procedures. Generally speaking, an organ transplant last from 4 to 8 hours. In re-transplant cases it can take much longer, and complications are also more common.
What are the main risks we face in a transplant?
Transplantation is the most complex procedure in the clinical setting. Therefore, the risks are higher than in any other case. Bleeding and intraoperative cardiac arrest are the most feared complications. Bleeding is more common in patient with previous coagulopathy, severe portal hypertension, and re-transplantation. The cause of cardiac arrest is multifactorial, and is related to previous patient conditions and severe intraoperative bleeding.
Will the transplant affect the reproductive system?
Expectations?
You may expect your child to have a normal life. However, the concept of normal life differs considerably from one to another. They can attend school, play sports and spend time with friends. When quality of life is assessed, the perception of parents is usually worse than the perception children have about their own life.
Complementary links
– Medline Plus: Organ transplantation
– Organdonor: Transplant Process
– Wikipedia: Organ transplantation
– Better Health: Organ and tissue transplantation
– United Network for Organ Sharing: Organ transplants, what every kid needs to know
– NCBI: Who needs a transplant and when?
– Organdonor: Organ Donation Statistics
– NCBI: WHO: Human Organ Transplantation
– Cleveland Clinic: Organ Donation and Transplantation
– NCBI: Why is organ transplantation clinically important?
– HealthDirect: Organ transplants
– United Network for Organ Sharing: How does UNOS save lives?
– WebMD: Common Health Problems After an Organ Transplant
– MedlinePlus: Transplant rejection
– Wikipedia: Transplant rejection
– Tattoos and piercings after a transplant
– Health24: What is the lifespan of 4 common organ transplants?
– Wikipedia: Immunosuppressive drug
– Healthline: About Immunosuppressant Drugs
– United Network for Organ Sharing: Types of immunosuppressants
– Donate Life California: Explaining donation & transplantation to children